This makes me REALLY cross!
It’s not about bouncing back… it’s about moving forward.
A word of warning – I am about to get on my soapbox here. Many of you will know that once I do that, I find it very difficult to get off it! ![]()
The ‘bounce back’ message makes me cross – REALLY cross ![]()
This message is putting an immense amount of pressure on women.
Have you seen (yet another!) picture of a mum at 6 weeks post-natal with a flat tummy? Is she back to working out at a high level? Does she look radiant and well-slept? Is she really back to lifting the same weight at the gym?
![]() Where are the pictures of the mums that haven’t managed to get out of their pjs (and it is 5pm)??
Where are the pictures of the mums that haven’t managed to get out of their pjs (and it is 5pm)??
![]() What about the women who go 5 days without washing their hair? (I was this person in the early weeks after having my boys…)
What about the women who go 5 days without washing their hair? (I was this person in the early weeks after having my boys…)
![]() What about women who have less support at home? Do their partners/husbands work away?
What about women who have less support at home? Do their partners/husbands work away?
![]() What about single mums? Will those mums be back to training within a few weeks of having their baby?
What about single mums? Will those mums be back to training within a few weeks of having their baby?
Also – are women who are feeling vulnerable and self-conscious likely to be posting images of their bodies all over social media?
No, probably not…
Maybe you are only seeing a very small proportion of women… Also, how many photos have been taken before they found the one that gave the best view of them? Is it ‘touched up’? Maybe ![]()
Before you are self-critical about your body, ask some questions about what you are seeing…
How many mums out there are REALLY bouncing back??
Everybody out there has a different journey. It is not about looking left and right at what others are doing – it is YOUR journey, and it is about putting 1 foot in front of the other.
Give things time and take the pressure off yourself. If it is a priority for you, you will get back to what you love, whether it be the gym, running, HIIT training, weightlifting, playing sport….
Do it on your own timescale, there is no race to the finish line.
For now, be kind to yourself ![]()
What should I look out for when choosing a Pelvic Floor Physiotherapist?
I have had a few emails and messages recently from women who don’t live in the area (I’m based in Cheshire) and want to find a Women’s Health Physiotherapist close to them.
I thought it would be useful to write my thoughts in a blog for anyone who might need it.
There are a few things to consider:
- This might sound obvious, but make sure the physiotherapist that you chose has skills in internal examination and treatment. There are physios out there claiming to treat pelvic floor conditions without doing internal assessment. Internal assessment is really important if you have pelvic floor problems – how else do you know what’s happening down there if it’s not assessed?
- Experience – it is usually best to choose someone who has been working in the specialism for a long time. Experience brings knowledge, and knowledge brings better care and treatment. I have been working in the specialism for over 10 years and have assessed and treated hundreds of women, but I’m still learning every day. It’s a complex area and you need to be sure your physiotherapist is highly skilled to allow you to have the best assessment and treatment.
- What is your end goal? How important is this goal? Think about this and talk to your physiotherapist about it at your first session. For example, if you want to be able to run a marathon without bladder leakage you need to discuss this at the first session! Will the physio work with you to help to try and reach this goal?
- You need to be sure you are comfortable with your physio. So often, the women that attend my clinic talk about the importance of ‘clicking with their physio’. If you are having issues with your pelvic floor, you will be discussing some really intimate things and you will be likely to have an internal examination. It’s always a good idea to check the physio out before hand – look at their website, check their social media page (if they have one), talk to others who might have been to see the physio. Call the physio if you want to have a chat with them before considering booking in. Get a feel for them because it needs to ‘feel right’! (In my experience, most pelvic floor physiotherapists are lovely though!)
- Virtual appointments – appointments over video have become common practice with the recent COVID-19 pandemic. You may now find that a lot of pelvic floor physiotherapists are offering these as well as face-to-face sessions. Yes, a pelvic floor examination cannot be done over video (and yes an examination is really important as I have already said!), but there are quite a few things that can be achieved over video. So perhaps think about a virtual appointment if you really want to have a session with a particular physio. That way you could literally see any physio in the world!
The magic that occurs 6 weeks after having your baby… or does it?!
“I’ve had my 6 week check… I’m good to go”
Many women are eager to exercise after having a baby. Is your driver the headspace that exercise gives you? Perhaps you are an athlete and you normally pursue exercise at a high level? Is it to help shift baby weight? Perhaps you have been comparing yourself to other mums? Scrolling through Instagram and seeing yummy mummies with amazing bodies doesn’t help with this…
Whatever your motivation to get back to exercise, more and more women are wanting to exercise soon as they can after childbirth. And do you know what, I completely get it. I have been there 3 times myself after each of my boys were born. For me, the major drivers were getting ‘me time’ back and getting that endorphin release.
Just last year, guidelines were published offering guidance on returning to running after having a baby. The guidelines were welcomed by a lot of people – me, other Women’s Health Physiotherapists, fitness professionals as well as mums themselves! I use these guidelines as a framework which very much underpins my practice.
One thing I can say is that it is impossible to give a timeframe for return to exercise that suits ALL women – we are all different, we have all been on a different journey, we all have different bodies, and we will all have different exercise goals. As a Specialist Women’s Health Physiotherapist, I have been assessing, treating and advising postnatal women for many years. I get asked these questions time and time again:
“When can I exercise again?”
“How should I build up my exercise up?”
“What exercises or movement should I avoid, if any?”
“Can I now do sit ups?”
“Am I allowed to do impact exercise?
“Can I do weight-lifting?”
If a post-natal mum asks me a question like this, I cannot answer it accurately unless I fully assess her. Without an assessment, it is impossible to give clear individualised advice. One size DOES NOT fit all!
Physiotherapy Assessment
So, if a woman wanting to return to exercise comes to clinic, what happens in order for me to give her the individualised advice that she needs? I carry out a ‘subjective assessment’ where I ask a series of questions:
- What kind of exercise do you want to do?
- Have you previously exercised?
- What level do you want to get to with your exercise?
- What was the mode of delivery – vaginal delivery / caesarean section?
- Give me your birth story…
- Were there any complications? If so, what were these?
- Are you breastfeeding?
- How are you feeling since having the baby? Are you having any problems?
- Are you having any urgency or leaking from your bladder or bowel? Do you have any heaviness down below?
- Do you have any other health problems / concerns?
These are just some of the questions I will ask. I use her answers to build a clear picture of the person sat in front of me.
Clearly all women will have a different story and will have different answers. Following on, I would carry out a thorough physical examination (‘objective assessment’). This would include assessing:
- Posture and action of the diaphragm
- Relevant functional movements and sport specific tasks for that woman
- Strength and flexibility in the muscles around the hip, back and pelvis
- Function of the abdominal muscles, including diastases recti
- Pelvic floor muscles – including contraction, relaxation, co-ordination, endurance AND strength
- For possible pelvic organ prolapse
- The attachments of the pelvic floor (during some vaginal deliveries the pelvic floor muscles can lose some of their attachment to the bones of the pelvis)
- The size of the opening in the pelvic floor (the medical term for this is gh+pb)
It takes around 90 minutes to complete an initial assessment. Most women then require treatment and rehabilitation over several appointments to ensure a safe return to post-natal exercise.
The risks of an early return to exercise…
So, what are the risks of a return to exercise too early? Pelvic organ prolapse, bladder problems, bowel problems, pain, worsening diastasis recti – just to name a few…
The ‘6 Week Rule’
Most women follow the standard ‘6 week rule’ and resume after their post-natal GP check. Sadly, few women actually receive a thorough assessment of their body at their GP check and are often just told that they can resume exercise.
I believe the ‘6 week rule’ can be harmful. It puts all women into the same bracket. It assumes that your body has healed, that you know how to build up / adapt / change / return to your exercise of choice. It also assumes that that all deliveries and recoveries are the same, that all women’s bodies the same and that all women are returning to the same activities.
Let’s think about a runner who has broken her ankle. Typically, her leg will have been placed in a cast, she will have been told to use crutches and will have probably been told not to weight bear on it for 6 weeks. She sees her doctor at 6 weeks and the cast is removed because her bone has heeled back together. Does she at that point start running right away? Of course not! She will follow a progressive rehabilitation programme to get back to running. This is often under the guidance of a physiotherapist. The physiotherapist will treat, guide and direct the athlete working on flexibility, strength and function. After a period of time (typically 3-6 months after the initial injury), she will be able to safely get back to running knowing that she has the strength and flexibility to do it.
So why is pregnancy and childbirth any different? No matter how ‘simple’ the birth is; there is major trauma to the pelvis, pelvic floor and abdominal muscles. Why are women not given the same attention and rehabilitation as an athlete with an ankle injury. This completely baffles me!
Finally…
In summary, there is no magic that happens at 6 weeks. Each and every post-natal woman (especially one wanting to resume exercise!) needs to have a thorough individualised assessment with a Specialist Women’s Health Physiotherapist. This assessment needs to take account of her exercise goals, her body and her birth journey in order to guide her back to exercise safely.
Do you have a ‘mummy tummy’?
A mummy tummy is that frustrating post-baby pouch that doesn’t seem go away. It can even sometimes lead to that dreaded embarrassing-for-all “when are you due?” question. One of the most common questions I am asked is whether I can offer any help with this very common issue.
I find that there are generally two ways women react to their post-pregnancy tummy:
- Embrace their new body shape, accepting that they have grown a baby and of course their tummy won’t ever look the same.
- Feel really uncomfortable and take a huge knock in self-confidence. They are generally prepared to do anything possible to return their tummy back to how it used to look.
Yes, there are some women out there who appear to bounce back immediately, and their stomach will look flat and fabulous 3 days after pushing their baby out (I know, not fair…), but there are many others who just cannot seem shift that mummy pouch!
What causes ‘mummy tummy’?
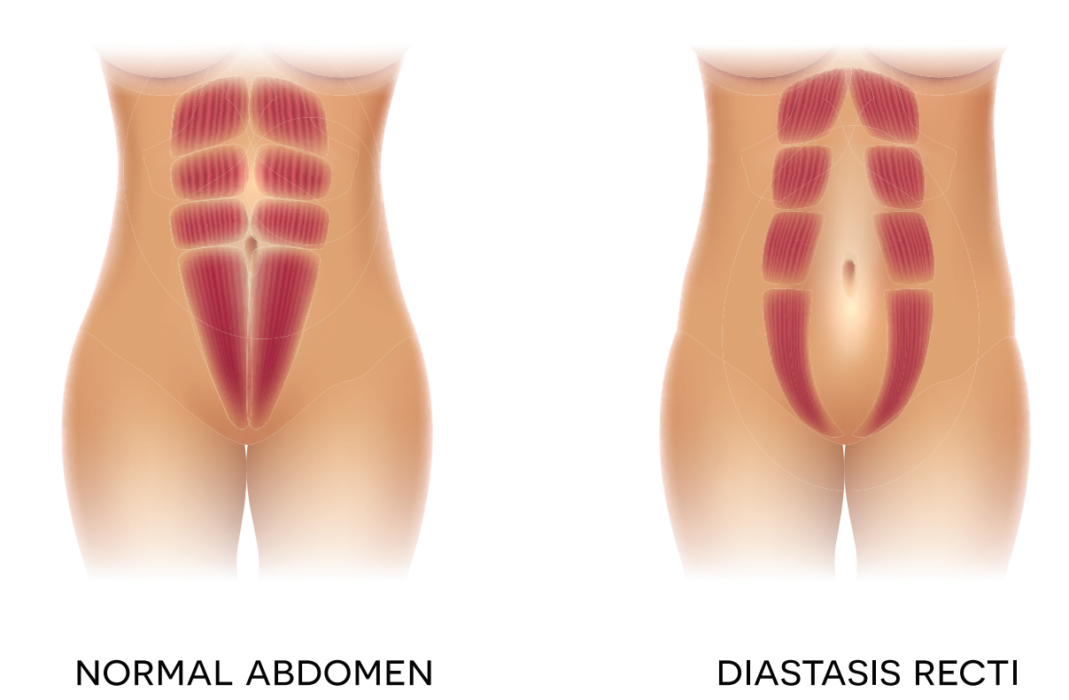
So let’s look at what’s going on with our bodies. During pregnancy, the growing uterus stretches the muscles of the abdomen. This causes the rectus abdominus (6 pack muscle) to separate in the middle – a condition called diastasis recti or diastasis recti abdominus. In this condition, the linea alba elongates and becomes thinner.
All women have some degree of diastasis in pregnancy. Every woman is unique and will have different degrees of separation in their rectus abdominus muscle. It is important to know that it is a normal occurrence which allows the abdomen to expand to accommodate a growing baby.
So, if it’s normal and it happens to all pregnant women, do we then just accept it? Embrace it? Hide it? Wear baggy tops forever?
Can physiotherapy help?
Yes!
After you have given birth to your baby, there will be some natural healing and coming together of the rectus abdominus muscles. Research has found that this natural healing will occur in women up to 8 weeks post-natal. For this reason, I usually suggest that women wait 6-8 weeks to see me. This allows the body some time to heal naturally.
I do lots of things to help treat diastasis recti. The most important element is a bespoke exercise programme to address individual needs. Every woman is different and there is no optimal one size fits all approach. Each woman needs a different programme to target their own split most effectively.
Good nutrition and hydration are also extremely important to facilitate tissue healing. Both of these are therefore discussed during your physiotherapy sessions.
How do you measure or check your split?
It can be tricky to assess yourself. Ideally, an assessment should be carried out by a Specialist Women’s Health Physiotherapist.
There are a number of things to measure and consider when carrying out an assessment. To accurately assess the separation, your physiotherapist should check 4 things:
- The width of the split
- The depth of the split
- The tension of the linea alba
- The vertical separation
Your physiotherapist should also assess your diaphragm (breathing), pelvic floor, posture and other abdominal muscles. These are all interrelated and equally important parts of the puzzle in the assessment and healing of diastasis recti.
So, if you are worried about your ‘mummy tummy’ and want to do something about it, you are not alone. Don’t suffer in silence. Book in today and let me help.
Babs is a Specialist Women’s Health Physiotherapist with 15 years’ experience. She set up Female Focus in 2018 with the aim of providing women with that gold standard care that that they deserve in pregnancy, birth and beyond. She has 3 boys herself, therefore can speak from both personal and professional experience.
Want to improve your sex life this Valentine’s Day?
Want to improve your sex life? Getting your pelvic floor muscles stronger may just do the trick!
Valentine’s day is billed as the most romantic day of the year and many people are looking for ways to spice things up in the bedroom. Though it may seem simple, strengthening your pelvic floor muscles could be the best way to bring some extra spark into your sex life.
Where are your pelvic floor muscles and what do they do?
Both men and women have pelvic floor muscles. These muscles are located at the base of your pelvis, stretching from your pubic bone at the front to your tail bone at the back. They have 3 main functions for women.
- They keep your bladder, womb and bowel in the correct position – preventing pelvic organ prolapse
- They tightly close your bladder and bowel openings to prevent incontinence
- They help with sexual function and sensation
We’re focusing on the final point ?
So what’s the issue?
In a recent study, it was found that over 60% of women suffer with some sexual dysfunction in the first year following childbirth. This may manifest itself differently for each woman. The most common issues are a loss of libido, pain during intercourse and an inability or reduced ability to achieve an orgasm. Understandably, these are sensitive issues and few women are comfortable discussing them openly. Unfortunately, this mean that most women do not realise that these problems are so common. Specialist physiotherapy can help, but most women do not know that this help is available.
The vaginal walls are layered with pelvic floor muscles. Studies have found that when a woman climaxes her pelvic floor muscles elicit a strong contraction (or several contractions). Strengthening these muscles by giving them a regular work out may therefore improve your orgasms! In a recent review it was found that pelvic floor muscle exercises alone improved sexual desire, arousal, orgasm and satisfaction in the post-natal period.
It takes time to strengthen your pelvic floor muscles. Like any other muscle in your body, you need to work the muscles correctly and regularly in order to strengthen them. Not only do you want stronger muscles, you also want physically bigger muscles of the pelvic floor – the aim is to get ‘ripped’ down there! It usually takes around 4 months (at a minimum) to see significant improvements.
How do I work my pelvic floor?
- Sit or lie comfortably
- Imagine that you are trying to stop yourself passing wind from your back passage. Now imagine you are trying to stop the stream of urine at the same time. You need to think of squeezing inside your vagina. You should feel your muscles lift up and squeeze tight.
- Think “tailbone, pubic bone, together and lift”
- Try to contract your pelvic floor muscles when you exhale (or breathe out).
You need to practice long squeezes to build up muscle endurance and short squeezes to enable the muscles to react quickly. Ideally, you should be able to tighten, squeeze and hold pelvic floor muscles holding them for 10 seconds, repeating this 10 times in a row. You should then follow with 10 quick squeezes.
The aim is to complete this process 3 times each day. Be patient – it may take time for you to be able do this! As you improve you will notice that you can hold your squeeze for longer and do more repetitions.
In order to ensure that you achieve a ‘perfect’ contraction (or an isolated pelvic floor contraction), try to:
- Avoid pulling your stomach in excessively
- Avoid squeezing your legs together
- Avoid tightening your buttocks
- Avoid holding your breath
A feeling of gentle tightening in your lower abdomen is normal.
Can my pelvic floor get too strong?
Strength is important, YES, but so too is relaxing your pelvic floor. If you are experiencing pain during sex it may be an indication that your pelvic floor muscles are not relaxing properly (known as pelvic floor over-activity). If this is the case, try to practice some relaxed breathing regularly during the day (and before intercourse) to see if this helps with your pain.
Thanks for the information. So what’s next?
So, let’s say that you are aiming to get strong down there……. But how do you know if you are contracting your pelvic floor muscles correctly? And on the flip-side, how do you know if you are able to relax them?
Unfortunately, research has found that only half of women contract their pelvic floor muscles correctly. You can try to check your own pelvic floor contraction by inserting your finger into your vagina. You should be able to feel the vaginal walls gently tighten around your finger when you exercise your muscles. Alternatively, ask your partner if they can feel your vagina tighten during sex when you contract your pelvic floor muscles. You should also be able to fully ‘let go’ of your pelvic floor contraction. This is important as it ensures that your pelvic floor muscles can fully relax.
If you are unsure, an assessment with a Specialist Women’s Health Physiotherapist will tell you if you are doing the right thing, and if you are not, how this can be corrected. Your physiotherapist can also give you a progressive exercise programme to help you build up (or relax) your pelvic floor muscles in the best possible way.
…for now, Happy Valentine’s Day to all you lovely ladies and happy squeezing! ?
Are we failing to care for mums?
Inspired by a rare chance to lie on the sofa full of turkey, chocolate and vino, it feels like a good time to write my first ever blog. How exciting!
My three beautiful boys – aged 2, 4 and 5 – are currently wrestling on the carpet. This is standard behaviour for these three. I have just said “Somebody is going to get hurt…” for the 90th time today. They ignore me (as usual) and continue to wrestle.
Anyway…I can’t believe that I grew these boys inside my body. It really is unbelievable when you think about it. My uterus has grown to the size of a watermelon three times to house these boys. Yes…I know, women are ‘made’ to give birth. After all, each of us has a vagina, a uterus, ovaries blah blah blah.
Do our bodies bounce back after having a baby? Erm…NO! Firstly, you grow a seed, which turns into an apple, which turns into a grapefruit, which eventually turns into watermelon. You then either push that watermelon out of your vagina (usually tearing it in the process) or have it cut out of your tummy via a huge incision through your abdominal muscles. What planet are we on if we think our bodies will just bounce back to normal (especially if we do it more than once)?
In short, women need guidance and rehabilitation following pregnancy and childbirth. This happens in France as standard for every new mother, but not in the UK. After a traumatic knee injury or surgery, you would expect physiotherapy to help you to regain movement, strength and normal function. Why not following childbirth? It’s pretty mind boggling.
I have pondered this over the years working as a Specialist Women’s Health Physiotherapist in the NHS. Very simply, I think it comes down to three main reasons:
- Women have been giving birth ‘since the dawn of time’. We are under the impression that our bodies are built to do it and to cope with the after effects.
- The impact of pregnancy and childbirth on the mother is (much to my frustration) rarely discussed and quickly forgotten. Our beautiful babies receive all of the care and attention.
- Healthcare professionals do not tackle and often normalise postnatal problems such as leaking. This in turn leads to women accepting these problems as normal and something they just have to live with.
Here are the stats…
A huge 50% of women who have had children will have some degree of pelvic organ prolapse (Hagen & Stark 2011). Some women may not even know they have one.
In one study, the prevalence of incontinence and intravaginal prolapse was 42% in women with one or more vaginal deliveries as opposed to 35% in women who had a C-section delivery (Sakala 2006). From this we can conclude that having a C-section reduces the chances of having pelvic floor problems, but in no way eliminates them.
It has been found that the gap between the rectus abdominus muscle does not change without intervention 8 weeks after childbirth (Coldron 2008).
So why see a physiotherapist…
A women’s health physiotherapist is the only healthcare professional out there who can accurately assess and retrain pelvic floor muscles. At the same time, they can also assess and retrain breathing, posture and the abdominal muscles.
When you start to train a muscle (or a group of muscles), any strength gains you make during the first few weeks are mostly due to simply learning how to actually contract the muscle you are exercising/recruiting. It is only after a few weeks / months of sustained training do your muscle cells start to get bigger, a process called “hypertrophy” (Jones et al 1989).
Retraining muscles after injury is essential as inhibited muscle does not automatically reactivate and retrain. In other words, if you don’t retrain damaged muscles the chances are they won’t do it themselves.
All of this leads me onto my soapbox……
I believe that EVERY single woman that has had a baby should have an assessment with a Specialist Women’s Health Physiotherapist. Are we failing to care for mums? Absolutely.
My mission at Female Focus is to change this. I am a qualified Mummy MOT Practitioner. This means that I can offer a specialist postnatal examination for women following both vaginal and caesarean deliveries. A Mummy MOT will assess how your posture, pelvic floor muscles and stomach muscles are recovering after birth. And if they’re not, you can be provided with exercises and treatment to help you in your recovery. It is never too late to have a Mummy MOT and rebuild your foundations, whether you had your baby 6 weeks ago or 40 years ago.
Hope to see all you mums soon. For now, Happy New Year! Time to get back to our beautiful children.




Recent Comments